PRESENTATION TO WAKEFIELD COUNCIL’S
OVERVIEW AND SCRUTINY COMMITTEE
THE CASE AGAINST WATER FLUORIDATION
January 2016
Author: Joy Warren, BSc. (Hons) Env. Sci.
Coordinator, UK Alliance Opposed to
Water Fluoridation

“If this stuff gets out into the air, it’s a pollutant; if it gets into the river, it’s a pollutant; if it gets into the lake, it’s a pollutant; but if it goes right straight into your drinking water system, it’s not a pollutant. That’s amazing.”
Source: Dr J. William Hirzy (May 1999), former Senior VP of Chapter 280 of the National Treasury Employees Union and Senior Chemist at the U.S. Environmental Protection Agency Headquarters.
Executive Summary
This report initially deals with the statistically insignificant findings of the Bedford Dental Health Impact Study for five-year-olds and which was presented to Bedford’s O&S Committee in November 2015.
Citing this PHE Report, we show that the case for fluoride preventing children’s tooth decay is weak. The statistical methods used to attempt to justify fluoridation are transparent and whilst the bar charts seem to show that dental decay has marginally worsened since 2009 when fluoridation ceased in Bedford Borough, the Confidence Level Indicators tell a completely different story: dental decay has not worsened since fluoridation ceased in Bedford in 2009. Moreover, throughout the report the author is at pains to explain that the results are not statistically significant.
In Section 2, we move on to discussing the worrying lack of morality and medical ethics implicit in the practice of water fluoridation
If fluoride is not essential for good teeth, is it harming us? Logically, Section 3 lists and summarises recent research which cautions us to apply the Precautionary Principle (Section 8) when considering any proposal to fluoridate the public’s drinking water.
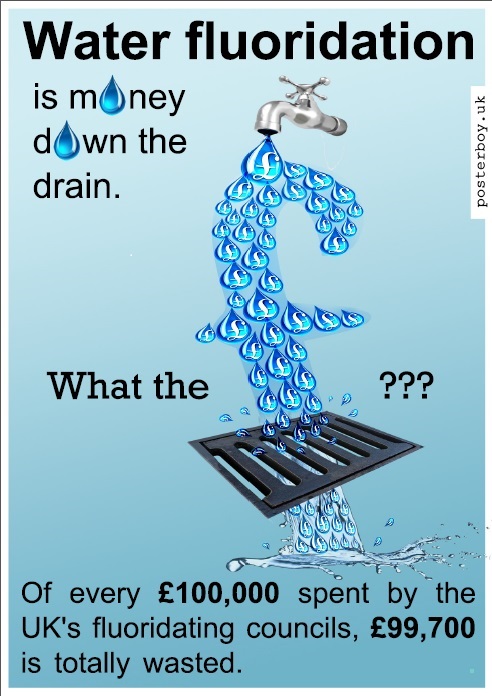
Another argument against fluoridation is the terrific waste of public money. Section 4 demonstrates that not only is a mere 4% of the acid drunk (with 96% being diverted elsewhere) but the amount of the huge capital outlay and ongoing revenue costs cannot be justified for the sake of making a tiny percentage of the fluoridating acid available to disadvantaged toddlers – the target group of fluoridation.
In Section 5 we review the causes of dental decay and conclude that disadvantaged small children are likely to disproportionately experience dental decay, often because of the neglectful and misinformed practices of their parents and guardians. We ask if it is equitable to expect entire populations to be fluoridated with a compulsory medicine for the sake of small children belonging to disadvantaged families which appear to be incapable of practising dental hygiene and providing nourishing food. Although we realise that it is Labour Party policy to care for people across all the social groups and reduce dental health inequalities, it was shown in 2000 and again in 2002, that the evidence base for a reduction in dental decay amongst disadvantaged families is extremely weak, contradictory and unreliable.
Section 6 explodes the myth that fluoride taken systemically reduces dental decay amongst fluoridated UK communities. At the time of writing, the British Fluoridation Society has published a particularly interesting piece of text which states that systemic fluoride is now understood to be the least important mechanism for preventing dental caries since it is the fluoride which is in the oral cavity which remineralises teeth and not the fluoride which is in the pulp cavity and dentine. Does this not imply that there is absolutely no need to fluoridate the fetus and the infant who have no teeth?
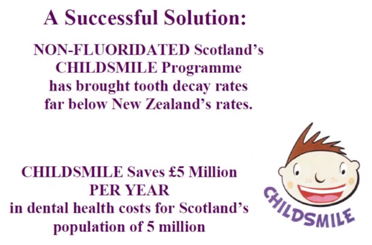
Effective alternatives to water fluoridation are available and Section 7 discusses how Scotland’s Childsmile programme is showing good results.
With so much controversy surrounding the practice of water fluoridation, the Working Group’s attention is drawn in Section 8 to the need to have regard to the Precautionary Principle.
We do not devote a section to summing up the conclusions. Instead, we have chosen to make the following statement:
It is counter-intuitive and medically unethical to impose a developmental neurotoxin on every individual living in Wakefield in the belief that fluoridation helps to remove dental health inequalities across social groups. This is clearly an erroneous belief as evidenced by the Open Letter to the Department of Health by the York Review Principle Researchers in 2002 (p. 23). We would like to point out that ‘belief’ is not ‘science’
Moreover, recent research, and in particular the Bedford PHE Report, has failed to make the case for systemic fluoride as a prophylaxis for the prevention of dental decay. Much dental decay is caused by factors which fluoride is ill-equipped to mitigate even if it were to be in contact with the surface of the teeth throughout the day and night. Surely it is the responsibility of those who promote fluoridation to conclusively prove that fluoride is effective. Despite this statement regarding its effectiveness being repeated ad nauseum by proponents, there is not one high quality piece of research which proves that dental decay is prevented by fluoride when taken internally. Eight years have elapsed since Wakefield last reviewed the issue and we are still awaiting conclusive proof.
Neither can we be convinced that fluoride is harmless in view of recent research which reinforces research which has been produced since the 1930s. We are acutely aware that fluoride was used as a highly effective treatment to dampen down over-active thyroid glands in the 20th Century and this fact on its own strengthens our certainty that fluoride has a role to play in the onset of the underactive thyroid. The cost to the NHS in treating hypothyroidism on its own is appreciable. But when we also have new research which indicates that ADHD is caused by fluoride, the cost to the NHS escalates. Removing fluoride – a developmental neurotoxin – would reduce NHS expenditure and make us a healthier nation. This is a goal to which we can all aspire. With alternative and available interventions for reducing dental decay – interventions which are targeted and sustainable – there can be no excuse to resort to ‘treating’ communities with a compulsory, hazardous by-product of industry which is heavily contaminated with heavy metals.
Section 1 A Critique of Public Health England’s (PHE’s) November 2015 Report on Dental Health as it Relates to Bedford’s 5-year-olds
We start this brief report with PHE’s November 2015 Dental Health Report because it is the most recent survey of 5-year-old children’s dental decay. Moreover, it concerns an unusual situation: in 2008, Bedford was fluoridated but in 2015 it was not fluoridated. We are thus provided with a before and after snap shot. The survey question was: has tooth decay increased since fluoridation ceased in Bedford in 2009?
Bedford Town and parts of Bedfordshire were first fluoridated in the 1970s at the request of the local Health Authorities. In those days, the public was not consulted. In 2009, Anglian Water suspended fluoridation of Bedford because their fluoridation dosing equipment at Manton Lane Water Treatment Works came to the end of its life. Again, the public was neither consulted nor informed. Nor was the Strategic Health Authority informed that Anglian Water had taken this unilateral decision. The cessation of fluoridation was discovered in 2012 by an activist who fights against water fluoridation and the news soon spread. Between 2012 and 2015, Fluoride Free Beds succeeded in setting up a useful dialogue with the Borough Council and the issue has been widely publicised within the Borough. Public Health England is anxious for fluoridation to resume in Bedford but has first to gain the approval of Bedford Borough Council which would be financially liable for maintenance costs. The issue is now before Bedford’s O&S Committee. At their most recent presentation to the O&S Committee in November 2015, Dr Feema Francis presented PHE’s report of the current state of oral health in Bedford. A comparison between the current dental health of non-fluoridated 5-year-olds and fluoridated 5-year-olds in 2008 is the main topic of the report.
One would have hoped that the Report would have provided substantive proof one way or the other regarding the efficacy, or otherwise, of systemic fluoride. Unfortunately, unless one applies a critical eye to the Report, the layman could be persuaded to believe that the dental decay has significantly worsened even though at 13 places in the text the authors state that their results are statistically insignificant! Wakefield’s Fluoridation Working Group is urged to study Bedford’s Report before reading the following critique.
~~~~~~~~~~~~~~~
The title of the PHE 2015 Report is “Dental health impact of water fluoridation in children living in Bedford Borough Council in 2008, 2009 and 2015”. The Report’s authors admit to only being able to provide statistically insignificant conclusions so it is very difficult to accept the use of the word “impact” in the title.
We are told that the report provides us with provisional results only. However, the data which were analysed by the Report’s authors cannot be provisional: it would not be ethical to analyse provisional data and to present the analysis in an authoritative report which is intended to persuade a local authority to introduce such a controversial health intervention.
Neither can the methods used to analyse the data be provisional since it is difficult to envisage why the authors would have used provisional methods of analysis when as professional statisticians, they would have opted for the best methods of analysing the data from the outset.
So, if the data is not provisional and the analytical methods for interpreting the data are not provisional, in which way is the Report provisional? Until and if we receive a revised report, we must accept this report as it stands and deal with it accordingly.
However, it is our considered opinion that the presentation of the provisional report on 10th November should have been delayed until PHE was satisfied that it had produced the final report.
How can firm decisions be made based on a provisional report and statistically insignificant conclusions?
In 13 places in the text, the results are described as being statistically insignificant. In other words, the researchers cannot demonstrate that dental decay has increased since fluoridation ceased in 2009.
Ref: pp. 1.4, 5.5, 5.6, 5.14, 5.21, 5.23 bis, 5.25, 6.1 bis, 6.3.1, 6.3.2, 6.4.1
Despite the slightly greater height of the coloured bars for 2015 in most of the bar charts, the confidence level (interval) bars ( I ) superimposed on most of the blue and red bars in the bar charts are more indicative of the true state of affairs than the height of the coloured bars. The I-bars display the minimum and maximum values in each data set (the range) and thus give a more accurate picture.
Compare this with the tops of the coloured bars. The tops represent the average (mean) or the centre value of each data set. Calculating the mean is a device often used by statisticians to influence the conclusions people make about the data.
In most of the bar charts in the Report, the I– bars for each pair of data overlap. Overlapping of the I– bars for the data sets for 2008 and 2015 means that no conclusions can be drawn from the data gleaned from the examination of five-year-olds’ teeth.
Fig. 1
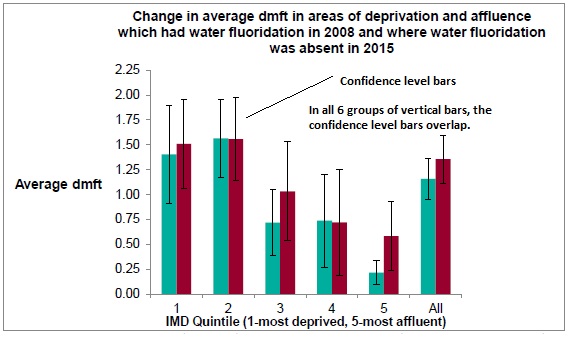
Where the confidence level bars overlap, no statistically significant conclusions can be assumed.
Ref: p. 21 of PHE’s Bedford 2015 Oral Health Report for 5-year-olds
Had the confidence bars in the pairs of data been in wide-spread positions and not overlapping (Fig. 2), then significant conclusions could have been be drawn from the data. For example:
Fig. 2
In order for the research findings to be significant, the confidence level bars must be separated by space between their lower and upper limits.
We are left with an uneasy feeling that although dental decay has not really increased in Bedford since 2008, Public Health England is not prepared to admit this. The Report is peppered with statements that the results were not statistically significant and yet in each of the summary sections it is claimed that there are differences between whatever is being measured in fluoridated and unfluoridated water areas. Those who are advised by PHE consultants have been primed to expect that there will be differences and the coloured bar charts seem to confirm that there are differences. But, the I-bars tell another story, viz. dental decay has not increased in Bedford since 2009.
So, to reiterate, PHE’s Report is remarkable in that it says two quite opposite things at the same time. It both agrees that fluoridation improves dental health, then disowns its own conclusions. This elevates it to an entirely new level of absurdity.
The bottom line is this: both the York Review and the Cochrane Collaboration Reviews of Water Fluoridation concluded that the evidence base for the effectiveness of water fluoridation is weak. If it can’t be proven to work, it can’t have any beneficial effects. Any such effects that may appear in the analysis are an indication of faulty data or analysis. Any effects which are discovered, having tortured the statistics (i.e. pseudo analysis) are entirely meaningless.
If the statistics have to be tortured in order to try to prove something is true, then the fact that the torture has taken place proves the opposite. In this case, that systemic fluoride does not prevent dental caries.
Children in the upper income group seem to have had more dental decay than found in this group in 2008. But again, our eyes are drawn to the tops of the coloured bars when they should be examining the overlapping I-bars. Since this discovery is at odds with most of the received wisdom of dental decay being more prevalent in the most deprived quintiles, further research is required in order to (a) interrogate this increase, (b) determine the existence of confounding factors and (c) establish the reasons why these children’s carers seem to be failing their charges. It’s just not good enough to single out this social group and not investigate further.
Ref: p. 22, Figure 7, IMD Quintile 5
An interesting hypothesis has recently been published and this relates to the increase in dental decay in babies brought up in households where the parents smoke. Although it is postulated elsewhere that families in the most deprived group are more likely to smoke than families in the most affluent group, the inhalation of secondary smoke could be the reason for increased dental decay in the most affluent group sampled in Bedford in 2015. We are also aware that children with ADHD experience higher levels of dental decay. ADHD strikes at all families – and not only those in Qunintiles 1-3. More research is definitely required. Claiming that children in the upper income group are experiencing more decay because Bedford’s drinking water is no longer fluoridated would be an unsubstantiated claim.
Ref: Tanaka S. et al. (2015) Secondhand smoke and incidence of dental caries in deciduous teeth among children in Japan: population based retrospective cohort study BMJ 2015; 351:h5397 doi: dx.doi.org/10.1136/b…
Broadbent, J.M., K.M.S. Ayers and W.M. Thomson (2004). “Is attention-deficit hyperactivity disorder a risk factor for dental caries? A case-control study. Caries Res. 2004;38(1): 29-33
We appreciate the fact that all decisions have to be evidence-based and realise that this is why Wakefield’s Working Group is particularly anxious to review research which has been produced since 2007. However, it is too good an opportunity to miss to fail linking ADHD research from 2004 and from 2014 with research on second-hand smoke from 2015.
We are also aware that submissions to the Working Group have to be evidence-based. Appended below is an excerpt from Bedford’s JSNA.
Bedford Borough JSNA, Oral Health Recommendations
Ref: Bedford Borough JSNA, Oral Health www.bedford.gov.uk/h… |
Evidence-based medicine (EBM)
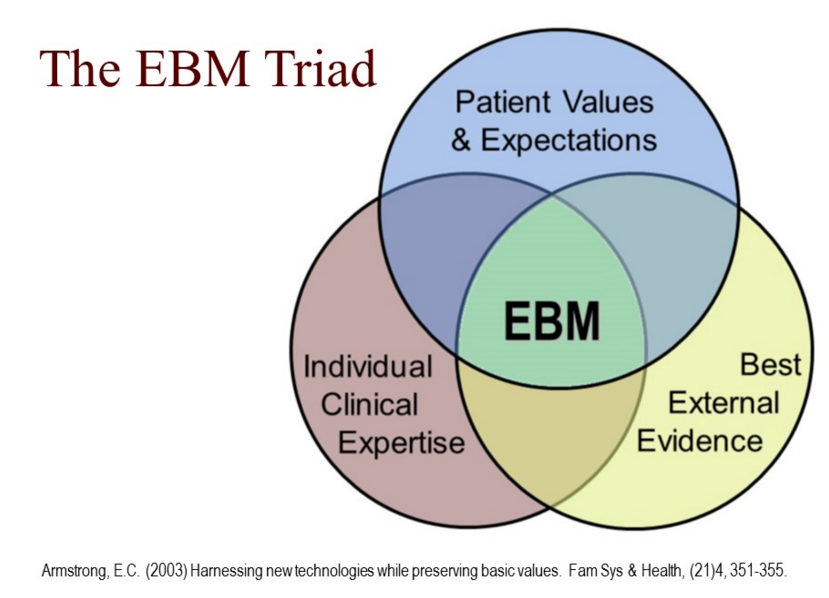
|
The concept of EBM is about making sure that when decisions are made they are made on the basis of the most up-to-date, solid, reliable, scientific evidence. In the case of medicine or health care, these are the decisions about the care of individual patients. “Evidence-based practice is the conscientious explicit and judicious use of current best evidence in helping individual patients make decisions about their care in the light of their personal values and beliefs.” What sort of evidence are we looking for? “Current best evidence”. Not perfect evidence – simply, the best there is. But not old or out-of-date evidence; we need to find modern, up-to- date current evidence.
How is this to be done? In a conscientious, explicit and judicious way. Again, the words are important. Conscientious – being careful, and thorough, in what you do Explicit – being “up-front”, open, clear and transparent Judicious – using good judgement and common sense
If you are going to practice in this way, you have to be able to find evidence from scientific studies that are relevant to your patients. You then have to understand those studies and be able to appraise them (not all studies will be relevant to your patient and even if they are, they may not be good studies). And finally you have to apply those results when making decisions about your patient. This means being able to integrate the evidence with your patients’ personal needs, their values, beliefs and wishes. |
Source: www.students4bestevi…
Evidence-based medicine needs to take into account patients’ values, beliefs and wishes. Since water fluoridation is a Public Health measure which is imposed on the masses, all the individuals who make up the ‘mass’ ought to be consulted about their values, beliefs and wishes before water fluoridation becomes decided. This is built into current fluoridation law for new schemes. But what a pity that the entire population of Wakefield might have to be involved in an expensive consultation when the decision not to fluoridate could be made painlessly by Wakefield Council at the outset. There would be very few residents who would be angry at not being consulted once the decision not to fluoridate had been made. On the other hand, we live in a democratic society so everyone should have the opportunity to take part in deciding on the issue.
This is where we are forced to examine the proposal from another angle. I, as a private citizen do not have the right to decide what medicine my neighbour takes. A group of citizens does not have the right to decree what medicines all the residents of a neighbouring housing estate should take. Yet, the nature of consultations forces this decision on us. Consultations are possibly not too problematical if they concern issues other than health but when we are dealing with something as outrageous as water fluoridation, consultations are clearly democratically unsound and highly unethical.
Even so, when asked to take part in fluoridation consultations, and once the issue is explained to them, the majority of respondents decline the offer, thus expressing their values, beliefs and wishes. The last time that a UK fluoridation consultation occurred was in 2009 in Southampton when of the 10,000 people who responded, 72% said ‘no’ to fluoridation. In the Isle of Man, the attempt to fluoridate the island came to nothing due to stalwart public opposition and without recourse to a consultation. At the beginning of time (i.e. 1952 when some towns in England were selected for the initial fluoridation trials), Andover threw out its Town Council, elected new Councilllors and forced a cessation to the trial.
Current evidence (Bedford’s Oral Health Report November 2015) shows that there is no statistically significant data to justify the re-imposition of water fluoridation on Bedford. At the moment, this is the ‘current, best evidence’ that we have. It is disturbing that it is self-proclaimed as being very poor evidence.
Perceptions of Dental Fluorosis
Bedford’s PHE report also provides 3 paragraphs on Dental Fluorosis and attempts to show that this disfigurement is of scant concern. We have copied the relevant data relating to Bedfordshire’s survey of Dental Fluorosis (which is not part of the Bedford PHE’s report) and compared the data with the Bedford Table at Section 5.26 (p. 24) of the Bedford PHE Report.
The first thing to note is that the term “Dental Fluorosis” is interspersed with the term “white marks”. According to the British Dental Association, PHE and the British fluoridation Society, Dental Fluorosis (DF) is a cosmetic issue. Attempts have been made in the past by the dental fraternity to make DF sound attractive. Indeed, according to them, there is nothing to be concerned about.
However, whilst the Bedfordshire data shows that 77 12-year-olds were aware that they had significant aesthetic opacities (also known as Moderate Dental Fluorosis), there is no attempt in the Bedford PHE Report to tell the O&S Committee how many Bedford 12-year-olds had significant aesthetic opacities. We are not even told the number of 12-year-olds who responded with “Yes, I have white marks” although it could be calculated but … that’s not the point. This data should be provided since it clearly exists. We have to ask why it has not been provided and why it has been air-brushed out.
White marks’ survey: Bedfordshire figures 2008-09
|
Population of 12-year-olds in Bedfordshire |
No. examined |
Yes, I have white marks |
No, I don’t have white marks |
Don’t know if I have white marks |
No answer |
Significant aesthetic opacities |
White marks not significant |
|
5,219 |
765 |
130 (17%) |
494 (64.6%) |
139 (18.2) |
2 (0.3%) |
77 (10.1%) |
156 (20.4% |
Source: www.nwph.net/dentalh…
White Marks’ survey: Bedford figures 2008-09
This data is contained in the data above – but some data is missing! Why?
|
Population of 12-year-olds in Bedford |
No. examined |
Yes, I have white marks |
No, I don’t have white marks |
Don’t know if I have white marks |
No answer |
Significant aesthetic opacities |
White marks not significant |
|
? |
240 |
(19.1%) |
(58.9) |
(21.6%) |
? |
? |
? |
Source: Presumably the same as for the Bedfordshire data set. The data set for Bedford has not been published on-line.
Significant aesthetic opacities (Moderate Dental Fluorosis) become more unsightly with the passing years until the ‘attractive’ white marks become ugly brown marks.
The Bedford Report’s conclusion that concern about fluorosis is very low is not corroborated by the Bedfordshire statistics where the children were asked specifically about significant aesthetic opacities and where 77 children stated that they had this significant disfigure-ment.
Twelve-year-olds are not in the best position to look into the future and worry about what their teeth will look like when they leave school. Once they’re 18 and working and if they don’t go to University/further education, they are no longer a statistic since any remediation of mottled teeth has to be paid for privately. Why ask 12-year-olds for their mental impression of future mottled teeth? We would get a more realistic reaction if we asked their parents. Be that as it may, 77 children seem to have been concerned and ticked the significant aesthetic opacities box meaning that 10.1% of Bedfordshire children were concerned. This is not “very low” and the gloss put on this disfigurement by Bedford PHE is completely unsupportable.
What is the purpose of this section of the PHE 2015 Report? Why is Bedford PHE trying to minimise the negative impact that Dental Fluorosis will have on these young people when they are adults?
Ref: Paras 5.26-5.28
Throughout the USA, approximately 41% of adolescents have Dental Fluorosis with 3% having moderate and severe DF. However, the percentage experiencing dental fluorosis in fluoridated areas is higher: 70-80%.
Marshall 2004; Locker 1999; Luke 1997
Dental Fluorosis negatively impacts enamel and dentine. Although the material out of which the teeth are made is differently mineralised, that does not imply that fluorosed teeth are stronger. Fluorosed teeth are difficult to drill and fill so future dental treatment promises to be more expensive for those affected.
Ref: Fejerskov O, Richards A, DenBesten P. (1996). The effect of fluoride on tooth mineralization. In: Fejerskov O, Ekstrand J, Burt B, Eds. Fluoride in Dentistry, 2nd Edition. Munksgaard, Copenhagen. pp. 112-152.
Fluoride can lead to cracks in tooth enamel, which can lead to decay beneath the enamel that often cannot be detected by a dentist using a probe. The subsequent result can be what appears to be a very minute amount of decay in the groove of a tooth which hides a ‘bombed-out tooth’ beneath it which is known in dental circles as a ‘fluoride bomb’. This is explained below in an extract from a journal article published in December 2007.
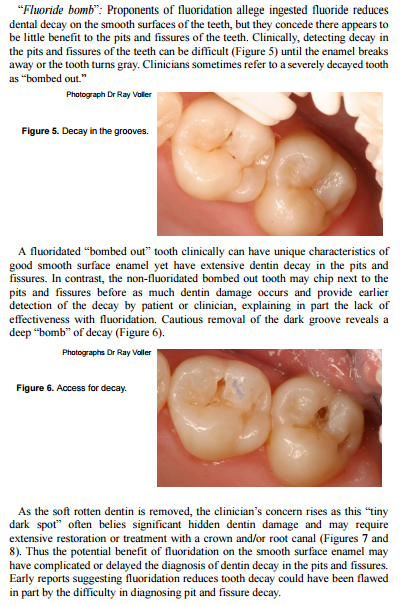
(Figures 7 and 8 not reproduced here.)
Section 2 The Moral and Medical Ethics’ Aspects of Compulsory Medicine

(Adapted from Blount, P.C. (1964). Compulsory Mass Medication: A Factual Guide to the Fluoridation Issue. London: The Clair Press.
For centuries, the men and women of Britain have enjoyed, as a right, the freedom to choose the form of medication they prefer for themselves and their children. That freedom is a precious heritage even though it may be taken for granted. The present proposal for adding fluoride back into Bedford’s drinking water after a break of 6 years means that we are being asked to surrender a part of that heritage and have a little of our freedom replaced by the dictator’s method of compulsion. Granted that it will be the benevolent Big Brother compulsion of Whitehall and not that of North Korea, but it will be dictatorship none the less!
An amazing number of red herrings have been drawn in written and oral debate on the subject of fluoridation, leading to much waste of time, heated argument and even derision and personal abuse of those who are against the idea of compulsory mass medication. Some people have confused both themselves and others by starting with the assumption that there is only one matter to be considered when, in fact, there are three – (1) the moral aspect of fluoridation, (2) the material aspect of fluoridation – including the medical, scientific, practical and economic considerations and (3) the legal aspect. If chairmen of committees would insist on these three aspects being dealt with separately, and in the order given, conclusions would be reached more quickly and with less friction.
The essence of the moral issue can be summed up in this question: Is it right, when no question of contagion is involved, to medicate people en masse, compulsorily, and in a manner which is objectionable to some? One does not need to go to doctors, dentists, water engineers, lawyers or any other specialist for guidance about this. One need go no further than one’s own conscience and an understanding of the Golden Rule of doing unto others as one would be done by.
In considering the moral aspect of fluoridation, the question of precedent inevitably arises. Once the principle of compulsory mass medication has been accepted, the individual will find himself deprived of a long-established right and the door will have been opened for all sorts of unpredictable things in the future.
Seeking to justify their case, the proponents of fluoridation argue that the precedent has already been established by the fact that many things are added to mains supplies of drinking water. If this is true, then they must say (a) precisely what these things are and (b) why they are being added. They will be led to the inevitable conclusion that all chemicals bar one (fluoride) are added to treat the water and not the consumer and thus there is no precedent. Moreover, even though it is true that compulsory mass medication is already being carried out in the country, this, in itself, would not seem to be a valid argument for extending the practice. On the contrary, it could be a very good reason for considering ways of bringing the practice to an end.
So much for the moral aspect of fluoridation. If having, carefully considered this aspect, one reaches the conclusion that it cannot be supported on moral grounds, that would surely bring one’s deliberations to an end, for no responsible person would support a measure which he considers to be unethical, no matter how attractive it might otherwise appear to be. If on the other hand, one reaches the conclusion that the practice of using mains water supplies as a vehicle for medication is ethical, then one must turn one’s attention to the material aspect.
Since no layman could possibly decide on the material aspect without guidance, he must turn to those specialists whose integrity, personal experience and first-hand knowledge of the issues involved qualify them to speak on the subject. Since these specialists are most divided in their opinions, the layman must then decide by which group he is going to be guided – those who are in favour of fluoridation or those who, for biological reasons, are against it.
If one does not mind taking risks with one’s own life and the lives of others against their wishes, then one may be prepared to accept the guidance of those specialists who are in favour of fluoridation. On the other hand, if one’s understanding of the Golden Rule causes one to be against taking risks with other people’s lives, then one will undoubtedly be guided by those specialists who are against fluoridation.
It’s as simple as that!
~~~~~~~~~~~~~~~~
NHS Constitution and Medical Ethics
Source: www.instituteofmedic…
The NHS Constitution states that individuals with ‘capacity’ can refuse all medical treatment advised by their GPs/Hospital Consultants.
”You have the right to accept or refuse treatment that is offered to you, and not to be given any physical examination or treatment unless you have given valid consent.”
Ref: www.gov.uk/governmen…, Respect, consent and confidentiality section.
The Chief Medical Officer (CMO) for England has a licence to practice as a GP. She has been told in the past that many people object to being given a medicine compulsorily in their water supply which is impossible to avoid. The names of 2000 objectors to compulsory mass medication have been provided to the CEO of the NHS at Richmond House since 2013 and the CMO has been advised that the CEO has these names.
To date, there has not been the courtesy of a reply from the CEO nor from the CMO for England. Why not?
One important medical ethic states that a medicine should not be prescribed beyond the time when the medicine is no longer required. So why is fluoride still being sponsored and prescribed via the NHS/DH for an illness which is neither contagious, neither effective for the prevention of dental caries in adult dentition when taken systemically, and which is not needed by people who have none of their natural teeth. Why?
Dental caries is not infectious across whole populations and therefore, PHE has no justification for insisting that this preventative medicine is ingested by everyone in a population.
Vaccinations are advised where there is infectious disease which affects whole populations. But thankfully, we are not subjected to mandatory vaccinations and we have the right to refuse vaccination. Parents also have the right to refuse for their children to be vaccinated. However, we cannot refuse to receive a prophylactic via our water supply. We are even taken to court if we refuse to pay our water charges if we object to being dosed with an unethical drug which we don’t need.
Section 3 Relevant Fluoride Research: 2007
1. <![if !vml]>![]() Peckham, S., D. Lowery and S. Spencer (2015). “Are fluoride levels in drinking water associated with hypothyroidism prevalence in England? A large observational study of GP practice data and fluoride levels in drinking water.” J. Epedemiol Community Health 2015; 0: 1-6
Peckham, S., D. Lowery and S. Spencer (2015). “Are fluoride levels in drinking water associated with hypothyroidism prevalence in England? A large observational study of GP practice data and fluoride levels in drinking water.” J. Epedemiol Community Health 2015; 0: 1-6
Summary: There was 30% more hypothyroidism in women aged 40+ living in fluoridated areas of England than in women of the same age living in non-fluoridated areas of England. There was almost double the amount of hypothyroidism in women aged 40+in the fluoridated West Midlands compared with women of the same age living in non-fluoridated Manchester.
This was an observational study. Although it didn’t examine individual women, each woman had had a diagnosis from her GP.
~~~~~~~~~~~~~~~~
2. Choi AL, Sun G, Zhang Y, Grandjean P (2012). Developmental Fluoride Neurotoxicity: A Systematic Review and Meta-Analysis. Environ Health Perspect :-. dx.doi.org/10.1289/e…
Summary: We performed a systematic review and meta-analysis of published studies to investigate the effects of increased fluoride exposure and delayed neurobehavioral development.
“The children in high fluoride areas had significantly lower IQ than those who lived in low fluoride areas,” write Choi et al.
After reviewing fluoride toxicological data, the National Research Council (NRC) reported in 2006, “It’s apparent that fluorides have the ability to interfere with the functions of the brain.”
Choi’s team at Harvard School of Public Health writes, “Fluoride readily crosses the placenta. Fluoride exposure to the developing brain, which is much more susceptible to injury caused by toxicants than is the mature brain, may possibly lead to damage of a permanent nature.”
Fluoride accumulates in the body. Even low doses are harmful to babies, to thyroid, kidney patients and heavy water-drinkers. There are even doubts about fluoridation’s effectiveness. New York City legislation is pending to stop fluoridation. Many communities have already stopped.
~~~~~~~~~~~~~~~~~~~~~~
3. Grandjean, P. and P.J. Landrigan (2014). “Neurobehavioural effects of developmental toxicity.” The Lancet Neurology, Vol. 13, Issue 3, Pages 330 – 338, March 2014
Summary: Neurodevelopmental disabilities, including autism, attention-deficit hyperactivity disorder, dyslexia, and other cognitive impairments, affect millions of children worldwide, and some diagnoses seem to be increasing in frequency. Industrial chemicals that injure the developing brain are among the known causes for this rise in prevalence. In 2006, we did a systematic review and identified five industrial chemicals as developmental neurotoxicants: lead, methylmercury, polychlorinated biphenyls, arsenic, and toluene. Since 2006, epidemiological studies have documented six additional developmental neurotoxicants—manganese, fluoride, chlorpyrifos, dichlorodiphenyltrichloroethane, tetrachloroethylene, and the polybrominated diphenyl ethers. We postulate that even more neurotoxicants remain undiscovered. To control the pandemic of developmental neurotoxicity, we propose a global prevention strategy. Untested chemicals should not be presumed to be safe to brain development, and chemicals in existing use and all new chemicals must therefore be tested for developmental neurotoxicity. To coordinate these efforts and to accelerate translation of science into prevention, we propose the urgent formation of a new international clearinghouse.
~~~~~~~~~~~~~~~~~~~~~~
4. Malin, A.J. and C. Till (2015) Exposure to fluoridated water and attention deficit hyperactivity
disorder prevalence among children and adolescents in the United States: an ecological association.” Environmental Health, doi:10.1186/s12940-015-0003-1. Article URL dx.doi.org/10.1186/s…
Summary: … this study has empirically demonstrated an association between more
widespread exposure to fluoridated water and increased ADHD prevalence in U.S. children
and adolescents, even after controlling for SES. The findings suggest that fluoridated water
may be an environmental risk factor for ADHD. Population studies designed to examine
possible mechanisms, patterns and levels of exposure, covariates and moderators of this
relationship are warranted.
Although another piece of research relating to ADHD that was published in 2004 is outside the scope of Wakefield’s Working Party’s brief, it is thought-provoking in the extreme. The 2004 research was a case-control study of children in Otago, South Island, New Zealand and explored the theory noticed in dental practices that suggested that children with ADHD tended to have a higher DMFT score than children without the condition.
“After controlling for fluoride history, medical problems, diet and self-reported oral hygiene, children with ADHD had nearly 12 times the odds of having a high DMFT score than children who did not have ADHD.” “No other factors were significant predictors. Dental practitioners and parents should consider ADHD to be a condition that may affect children’s dental caries experience.
Source: Broadbent, J.M., K.M.S> Ayers and W.M. Thomson (2004). “Is attention-deficit hyperactivity disorder a risk factor for dental caries? A case-control study. Caries Res. 2004;38(1): 29-33
This hypothesis is offered for consideration: if fluoride causes ADHD and if children with ADHD have a greater risk for dental caries, then the extra financial burden incurred in looking after ADHD children and in treating their dental decay could tip the scales and argue against the introduction of fluoridated water in an area. Even if it is not possible to conduct a survey at this time, the Precautionary Principle should be invoked (see Section 8).
~~~~~~~~~~~~~~~
5. Sawan RM1, Leite GA, Saraiva MC, Barbosa F Jr, Tanus-Santos JE, Gerlach RF (2010). “Fluoride
increases lead concentrations in whole blood and in calcified tissues from lead-exposed rats.” Toxicology. 2010 Apr 30;271(1-2):21-6. doi: 10.1016/j.tox.2010.02.002.
Abstract
Higher blood lead (BPb) levels have been reported in children living in communities that receive fluoride-treated water. Here, we examined whether fluoride co-administered with lead increases BPb and lead concentrations in calcified tissues in Wistar rats exposed to this metal from the beginning of gestation. We exposed female rats and their offspring to control water (Control Group), 100mg/L of fluoride (F Group), 30mg/L of lead (Pb Group), or 100mg/L of fluoride and 30mg/L of lead (F+Pb Group) from 1 week prior to mating until offspring was 81 days old. Blood and calcified tissues (enamel, dentine, and bone) were harvested at day 81 for lead and fluoride analyses. Higher BPb concentrations were found in the F+Pb Group compared with the Pb Group (76.7+/-11.0microg/dL vs. 22.6+/-8.5microg/dL, respectively; p<0.001). Two- to threefold higher lead concentrations were found in the calcified tissues in the F+Pb Group compared with the Pb Group (all p<0.001). Fluoride concentrations were similar in the F and in the F+Pb Groups. These findings show that fluoride consistently increases BPb and calcified tissues Pb concentrations in animals exposed to low levels of lead and suggest that a biological effect not yet recognized may underlie the epidemiological association between increased BPb lead levels in children living in water-fluoridated communities.
~~~~~~~~~~~~~~~~~
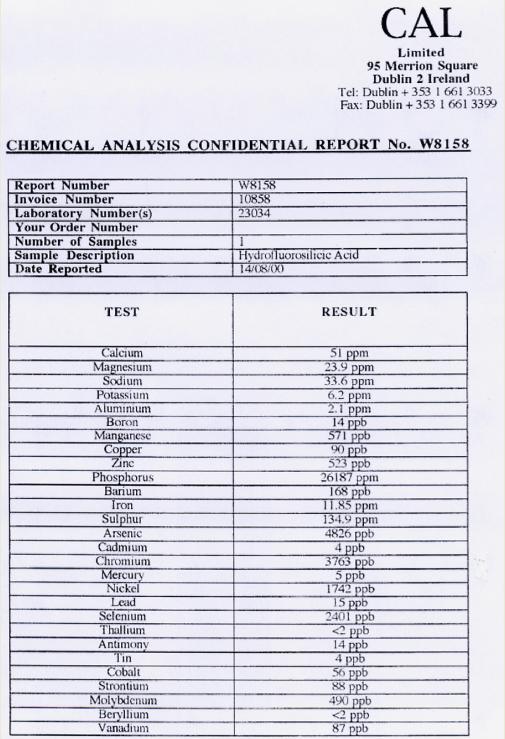
6. Mullenix, P.B. (2014). A new perspective on metals and other contaminants in fluoridation chemicals. International Journal of Occupational and Environmental Health. Volume 20, Issue 2 (April–June 2014), pp. 157-166
Summary: Fluoride additives contain metal contaminants that must be diluted to meet drinking water regulations. However, each raw additive batch supplied to water facilities does not come labeled with concentrations per contaminant. This omission distorts exposure profiles and the risks associated with accidents and routine use.
Metal concentrations were analyzed in three hydrofluorosilicic acid (HFS) and four sodium fluoride (NaF) samples using inductively coupled plasma-atomic emission spectrometry. Arsenic levels were confirmed using graphite furnace atomic absorption analysis
Results show that metal content varies with batch, and all HFS samples contained arsenic (4·9–56·0 ppm) or arsenic in addition to lead (10·3 ppm). Two NaF samples contained barium (13·3–18·0 ppm) instead. All HFS (212–415 ppm) and NaF (3312–3630 ppm) additives contained a surprising amount of aluminum.
Such contaminant content creates a regulatory blind spot that jeopardizes any safe use of fluoride additives.
7. Fluoride Action Network’s website section on reduced human and animal intelligence caused by fluoride exposure. (www.fluoridealert.or… ). To activate the links, click on them while pressing Ctrl.
Fluoride’s ability to damage the brain is one of the most active areas of fluoride research today. Over 300 studies have found that fluoride is a neurotoxin (a chemical that can damage the brain). This research includes:
Over 100 animal studies showing that prolonged exposure to varying levels of fluoride can damage the brain, particularly when coupled with an iodine deficiency, or aluminum excess;
49 human studies linking moderately high fluoride exposures with reduced intelligence;
34 animal studies reporting that mice or rats ingesting fluoride have an impaired capacity to learn and/or remember;
12 studies (7 human, 5 animal) linking fluoride with neurobehavioral deficits (e.g., impaired visual-spatial organization);
3 human studies linking fluoride exposure with impaired fetal brain development.
Based on this accumulating body of research, several prestigious reviews — including a report authored by the U.S. National Research Council, a meta-analysis published by a team of Harvard scientists, and a review published in The Lancet— have raised red flags about the potential for low levels of fluoride to harm brain development in some members of the population.
8. Cochrane Collaboration (2015). Water fluoridation for the prevention of dental caries. onlinelibrary.wiley….
Plain language summary
Background
Tooth decay is a significant problem worldwide affecting the majority of adults and children. Although levels of tooth decay have been decreasing in some communities (levels vary both between and within countries), generally children from poorer backgrounds (measured by income, education and employment) have greater levels of tooth decay.
Untreated tooth decay causes progressive destruction of teeth which is often accompanied by severe pain. This may lead to teeth having to be removed under local or general anaesthetic.
Fluoride is a mineral that prevents tooth decay. It occurs naturally in the soil, water and atmosphere at varying levels worldwide. Water can be artificially fluoridated (also known as community water fluoridation) through the controlled addition of a fluoride compound to a public water supply. Fluoridation is set at the ‘optimum level’, considered to be around 1 part per million (ppm).
Fluoride is also available in most toothpastes and can be provided as an extra preventive measure through products like mouth rinses, varnishes and gels.
An unwanted effect of fluoride use is the marking of permanent teeth (dental fluorosis) that is caused when young children, whose permanent teeth are developing, swallow excessive fluoride. This can range from mild white patches on the teeth to severe mottling with brown staining.
Review question
This review was conducted to assess the effects of water fluoridation (artificial or natural) for the prevention of tooth decay. It also evaluates the effects of fluoride in water on the white or brown marks on the tooth enamel that can be caused by too much fluoride (dental fluorosis).
Study characteristics
Researchers from the Cochrane Oral Health Group reviewed the evidence – up to 19 February 2015 – for the effect of water fluoridation. They identified 155 studies in which children receiving fluoridated water (either natural or artificial) were compared with those receiving water with very low or no fluoride. Twenty studies examined tooth decay, most of which (71%) were conducted prior to 1975. A further 135 studies examined dental fluorosis.
Key results
Data suggest that the introduction of water fluoridation resulted in a 35% reduction in decayed, missing or filled baby teeth and a 26% reduction in decayed, missing or filled permanent teeth. It also increased the percentage of children with no decay by 15%. Although these results indicate that water fluoridation is effective at reducing levels of tooth decay in children’s baby and permanent teeth, the applicability of the results to current lifestyles is unclear because the majority of the studies were conducted before fluoride toothpastes and the other preventative meaures were widely used in many communities around the world.
There was insufficient information available to find out whether the introduction of a water fluoridation programme changed existing differences in tooth decay across socioeconomic groups.
There was insufficient information available to understand the effect of stopping water fluoridation programmes on tooth decay.
No studies met the review’s inclusion criteria that investigated the effectiveness of water fluoridation for preventing tooth decay in adults, rather than children.
The researchers calculated that, in areas with a fluoride level of 0.7 ppm in the water, approximately 12% of the people evaluated had fluorosis that could cause concern about their appearance.
Quality of the evidence
The review authors assessed each study included in the review for risk of bias (by examining the quality of the methods used and how thoroughly the results were reported) to determine the extent to which the results reported are likely to be reliable. This showed that over 97% of the 155 studies were at a high risk of bias, which reduces the overall quality of the results. There was also substantial variation between studies in terms of their results.
Our confidence in the size of effect shown for the prevention of tooth decay is limited due to the high risk of bias in the included studies and the fact that most of the studies were conducted before the use of fluoride toothpaste became widespread.
Our confidence in the evidence relating to dental fluorosis is also limited due to the high risk of bias and variation in the studies’ results.
~~~~~~~~~~~~~~~~
9. These final three pieces of evidence predate 2007. They are included in the firm belief that the Working Group will not have been referred to them. Their existence is of great importance since they set the record straight.
a. The table below is US data which was used to justify fluoridation. It’s taken from Trendley Dean’s et al paper on “Domestic Water and Dental Caries including Certain Epidemiological Aspects of Oral L. Acidophilus.” Pub Health Report 54, 862-88, 24th May 1939. It is quoted in Exner and Walbott (p.115):
|
Towns in Illinois |
Fluoride in ppm |
Carious Permanent Teeth per 100 children |
Calcium in the water in ppm |
|
Galesberg |
1.9 |
194 |
62.2 |
|
Monmouth |
1.6 |
208 |
65 |
|
Macomb |
0.2 |
368 |
47.1 |
|
Quincy |
0.2 |
628 |
28.2 |
One’s eye is drawn to the first three columns which show that dental caries increases as the concentration of fluoride decreases. But there is another factor in this report – that of decreasing calcium correlated with increasing caries. We all know that calcium is good for teeth and that our bones and teeth are made of calcium. So which element reduces tooth decay? Fluoride or calcium? Perhaps it would have been a wiser Public Health measure to add calcium carbonate to drinking water in soft water areas?
~~~~~~~~~~~~~~~~~~~
b. We have referred to the 2015 research by Peckham et al of Kent University. The following information which is alluded to in the Peckham et al study is of relevance to the issue of hypothyroidism.
Hyperthyroidism, the euthyroid state and hypothyroidism are on a continuum:
<![if !vml]>![]() <![if !vml]>
<![if !vml]>![]() Hyperthyroidism The Euthyroid State Hypothyroidism
Hyperthyroidism The Euthyroid State Hypothyroidism
<![if !vml]>![]() <![if !vml]>
<![if !vml]>![]() Over-active Normal Underactive
Over-active Normal Underactive
From the evidence of medical practice of the 1930s – 1960s, we are told that an effective way of returning the over-active thyroid gland to normality was to give patients hot baths in which a carefully measured amount of a fluoride compound had been placed. Almost without exception, the treatment cured these patients. The fluoride was absorbed through the skin and served to dampen down the over-active thyroid. Some patients, however, were not so lucky since if the treatment continued past the point of the euthyroid state, they became ill with hypothyroidism. Worse still, the function of some of the patients’ thyroid glands was destroyed. It can be easily imagined that the initial difficulty was to accurately measure the volume of water added to a bath since baths vary in shape and size. Each time the patient bathed, he or she had to be accompanied by a medical practitioner to ensure that the exact amount of fluoride compound was added. It would also be important to time the duration of the bath. Because of their toxic nature, all fluoride compounds have to be handled with great care. The practice ceased when more convenient and more measurable drugs were developed.
We can now relate this medical practice to the discovery that women aged more than 40 in the fluoridated areas of England have 30% more hypothyroidism than their peers in non-fluoridated areas. The West Midlands shows an increase in hypothyroidism of almost double that diagnosed in Manchester. These days, it is not just bath water which contains fluoride. Fluoride is everywhere and in the most unexpected places. For example, Pepsi Max is made from a concentrate using Rugby town water which contains 1ppm fluoride. A “traditional cider” sold by Sainsburys contains 0.5ppm fluoride because although it comes from West Country apples, it is delivered to the food manufacturer as a concentrate and fluoridated water is then added before it is canned. Fluoride is in the cement used to attach implants, veneers and crowns. White fillings (glass ionomer) contain fluoride. Teeth whitening preparations, toothpaste, mouthwash, fluoride varnishes, dental milk, fluoridated salt, fluoridated toothpaste and dental floss all have a liberal sprinkling of fluoride. Food manufactured in fluoridated areas or imported fruit from the USA all contain fluoride because fluoridated tap water and fluoridated pesticides are used in the preparation and cultivation of foods.
Women who are deficient in iodide and who live in a fluoridated area and who are exposed to all or some of the products listed above, are more likely to experience hypothyroidism than those women who are not exposed to fluoridated tap water. So, it’s no wonder that the incidence of hypothyroidism is greater in fluoridated areas.
For a chronology of fluoride and the thyroid gland, go to: poisonfluoride.com/p…
~~~~~~~~~~~~~~
c. The Research Team Principals of the York Review (2000) wrote an open letter to the Department of Health in December 2002. The letter is appended here without amendment.
4 YORK SCIENTISTS’ OPEN LETTER
11th December 2002
Dear Minister,
We are scientists involved in the systematic review of evidence on the effects of water fluoridation, carried out by the NHS Centre for Reviews and Dissemination at the University of York. As far as we are aware, no other review of this topic is of comparable scientific standard, and we are concerned about some continuing misinterpretations of the evidence which could have implications for public policy. It is not for us to say whether the standard of evidence should be judged sufficient for a public health measure affecting whole populations, but we think it is important that decision makers are aware of what the review really found:
1. Effectiveness of fluoridation in reducing caries
We could discover no reliable, good-quality evidence in the fluoridation literature world-wide. What we found suggested that fluoridation was likely to have a beneficial effect, but in fact the range could be anywhere from a substantial benefit to a slight disbenefit to children’s teeth.
2. Effectiveness of fluoridation in reducing inequalities in dental health across social groups
This evidence is weak, contradictory and unreliable.
3. Safety of fluoridation
Apart from an increase in dental fluorosis (mottled teeth) we found no clear pattern among the possible negative effects we examined, and we felt that not enough was known because the quality of the evidence is poor.
We append relevant extracts from the report of the review from which the conclusions under 1. and 2. can be substantiated. 3. covers too broad an area to summarise easily.
Since the report was published in September 2000 there has been no other scientifically defensible review that would alter the findings of the York review. As emphasised in the report, only high-quality studies can fill in the gaps in knowledge about these and other aspects of fluoridation. Recourse to other evidence of a similar or lower level than that included in the York review, no matter how copious, cannot do this.
We think these matters are important enough to bring directly to your attention, as well as to the notice of others who have a stake in public health policy.
Yours sincerely,
(SIGNED) Professor Jos Kleijnen
Director, NHS Centre for Reviews and Dissemination
(SIGNED) Sir Iain Chalmers
UK Cochrane Centre
(SIGNED) Professor Trevor Sheldon
Head of Department
Department of Health Sciences, University of York
(SIGNED) Professor George Davey-Smith
Department of Social Medicine
University of Bristol
[Ref: www.appgaf.org.uk/ar… ]
[APPGAF is the All Party Parliamentary Group Against Fluoridation]
Section 4 How Water Fluoridation Wastes Money
<![if !vml]>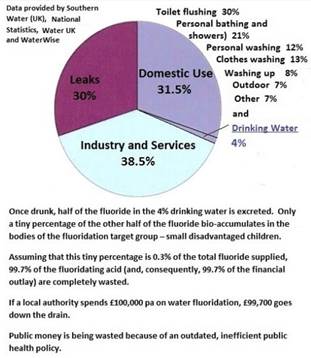
27.5% of fluoridated water used by households is not drunk by the family.
Only 4% of fluoridated water sold by fluoridating water companies is drunk.
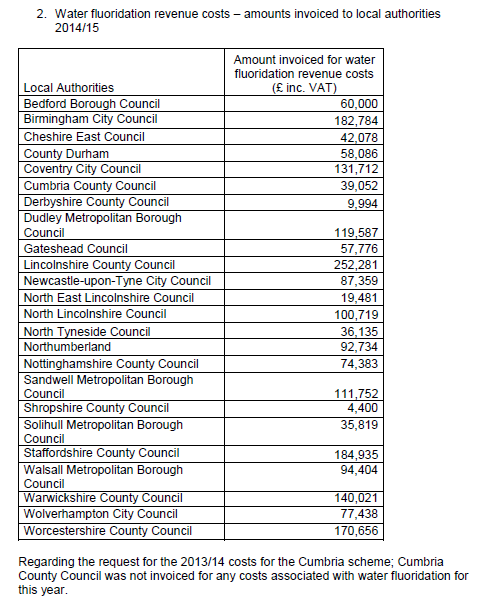
(The above figures were acquired by making a Freedom of Information request)
It is calculated that with a population of 331,000, Wakefield would have to pay PHE the sum of £140,000 pa for fluoridation revenue costs. Of this expenditure, approx. £138,000 pa worth of fluoridating acid and its supporting services would “go down the drain”. This would be an unjustifiable waste of money since it could never be a financially viable proposition to spend that amount of non-targeted money for the sake of a tiny percentage of disadvantaged tiny tots when targeted dental hygiene education would be far less expensive and effective.
The responsibility for initial capital expenditure (feasibility study and fluoridation equipment) would need to be negotiated with PHE.
Section 5 The Causes of Dental Decay in Disadvantaged Families
The following causes of tooth decay argue against the efficacy of fluoride in preventing dental caries. Even with fluoride in the water supply, dental decay continues to occur in fluoridated areas. (See Section 6 ). Fluoride is not a silver bullet.
Lead causes tooth decay
In research published in the International Journal of Environmental Studies (September 1999), Masters and Coplan studied lead screening data from 280,000 Massachusetts children. They found that average blood lead levels are significantly higher in children living in communities whose water is treated with silicofluorides [such as hexafluorosilicic acid]. Data from the Third National Health and Nutrition Evaluation Survey (NHANES III) and a survey of over 120,000 children in New York towns (population 15,000 to 75,000) corroborate this effect.
Masters and Coplan reported that some minorities are especially at risk in high SiF exposure areas, where Black and Mexican American children have significantly higher blood lead levels than they do in non-fluoridated communities.
Silicofluorides are used by over 90% of U.S. fluoridated towns and cities. Ironically, children with higher blood lead levels also have more tooth decay (Journal of the American Medical Association, June 23/30, 1999).
In certain towns and cities in the UK, there is a proportion of black and ethnic families. Such families are more prone to being damaged by silicofluorides, especially if they live in houses where the water pipes are made of lead. Also, certain poor areas of a town or city are close to contaminated land where children play.
Low calcium in soft tap water once weaned and poor calcium-deficient diets
Birmingham has soft water (total dissolved solids t.d.s 77) because the Elan Valley water which is piped to the city is soft with low levels of calcium carbonate. In the Republic of Ireland, much of the tap water is very soft (t.d.s 35). Disadvantaged families consume foods which are traditionally low in calcium. Calcium is an essential component of growing teeth and bones.
Baby-bottle decay (Early Childhood Caries)
It has been admitted by the dental fraternity that this type of decay could never be prevented by fluoride. Such decay is aggressive. Those on the Working Group, who are unaware of why early childhood caries is so aggressive, need to picture a toddler put to sleep with a bottle of sugary liquid on which it sucks for hours at a time.

Early Childhood Caries
The remineralisation of enamel in milk teeth cannot occur fast enough to prevent this type of decay.
Kissing the young child on the mouth
Being kissed on the mouth by parents or siblings once the first teeth have erupted can infect the young child with bacteria such as Streptococcus mutans. If dental hygiene in the family is not well observed, then the young child is more likely to experience dental decay.
Too much sugar/acid/phosphate
If young children don’t drink water, they will preferentially seek out pop (Coke, lemonade, Fanta, etc.) Such drinks are acidic and full of sugar or if Coke is the preferred drink, full of phosphoric acid which is more acidic than vinegar. In all cases, an acidic environment is generated in the oral cavity which encourages the erosion of enamel. If bacteria, such as Streptococcus mutans, are present in the oral cavity, decay will soon follow.
Regarding sugar, Dr Alison Tedstone, chief nutritionist for Public Health England, the Government agency responsible for tackling obesity, said: ‘Children are having too much sugar, three times the maximum recommended amount. This can lead to painful tooth decay, weight gain and obesity, which can also affect children’s well-being as they are more likely to be bullied, have low self-esteem and miss school. Children aged five shouldn’t have more than 19 grams of sugar per day – that’s five cubes, but it’s very easy to have more.’ (Ref: www.dailymail.co.uk/…
Poor enamel deposition (Amelogenesis imperfecta)
Some children are genetically unable to deposit a thick layer of enamel on their teeth. These teeth are prone to more rapid decay.
Dentine Bombs
This is explained on pp. 13-14. In brief, the dentine is decayed by bacteria entering through microcracks in fluoridated enamel and is not detected until the enamel overlying the decayed dentine caves in when it is probably too late to save the tooth.
The Connection between ADHD and Dental Decay
If fluoride causes ADHD (see p. 20), then it is counter-intuitive to fluoridate the young child which has ADHD. Research shows that fluoride is a developmental neurotoxin. It could be that fluoridated children with ADHD are not able to lay down robust tooth enamel due to the disruptive effect that fluoride has on their enzymes. The New Zealand research (2004 – see p. 20 ) points to children with ADHD experiencing alarming levels of dental decay.
Section 6 Worsening Dental Decay in Fluoridated West Midlands
All three newspaper reports appended below in full attest to the fact that the imposition of fluoride in the public water supply is not working to reduce dental decay. The apologists state that dental decay is on the increase because of there being a theory that decay figures are partially caused by increasing number of immigrants. However, if that is the case, then we need to see the proof. None has been forthcoming!
Coventry Observer, November 2008 (no longer accessible via the Internet)
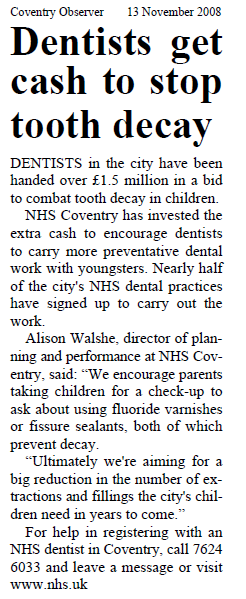
Coventry has been fluoridated since 1979.
Birmingham Mail, September 2011
Scheme piloted in Birmingham to boost children’s dental health
10:54, 15 SEP 2011
UPDATED 12:18, 14 OCT 2012
A TRIAL to boost children’s teeth is being pioneered in the region after it was shamed for youngsters’ rotting gnashers.

Dental issues
A TRIAL to boost children’s teeth is being pioneered in the region after it was shamed for youngsters’ rotting gnashers.
Nine dental practices in the West Midlands have been selected to look at ways of getting more children and other patients to see an NHS dentist by changing the way they are paid.
It comes after it emerged in June that a third of five-year-olds in Birmingham have rotting teeth with a mouth full of decay or fillings.
That was coupled with nearly 50,000 fewer city residents seeing an NHS dentist compared to five years ago when controversial changes to the dental contract were introduced.
Dentists are now paid for the amount of treatment they do but this trial by the Department of Health will see dentists paid for the number of patients they care for and the health results.
It will also include dentists promoting preventative dental treatments like fluoride varnish to prevent fillings.
Health Secretary Andrew Lansley said: “It is great to see that dentists in the West Midlands have signed up to be part of this important work.
“It will allow them to focus on promoting good oral health and preventing dental decay, rather than simply being paid to perform a series of procedures.
“It is vital that patients, and especially children receive high quality dental care, and the changes being trialled will mean dentists are paid according to the outcomes their patients see.”
Dentists selected to pilot the new system include Amblecote Dental Practice,in Dudley; Henry Road Dental Practice, in Yardley; Hillbrook Dental Health Centre, in Balsall Heath; South Road Dental Surgery, Stourbridge; West Park Dental, Smethwick and University Dental Centre, in Edgbaston.
There were 26,000 fewer children nationwide able to see a dentist up to June 2011, compared to the year up to March 2006 when the new NHS contract came in, according to the NHS Information Centre.
Patients struggling to register with an NHS dentist should call the dental helpline on 0121 465 1037.
Source: www.birminghammail.n…
Coventry Telegraph, 17th July 2014
‘Shocking’ increase in tooth decay in children in West Midlands
14:01, 17 JUL 2014
BY COVENTRY TELEGRAPH
300 per cent rise in youngsters in the region admitted to hospital for multiple teeth extractions

Tooth decay in children is rising rapidly in the West Midlands
There has been a 300 per cent rise in children in the West Midlands being admitted to hospital for multiple teeth extractions in what a senior dentist described as a “massive parenting failure”.
Some youngsters are undergoing hospital operations to remove all 20 baby teeth, according to Dr Nigel Carter, the chief executive of the Rugby-based British Dental Heath Foundation, who practises in the region.
Dr Carter said it “beggared belief” that a parent would not notice their child had a “mouthful of teeth rotten down to the gums”.
Figures revealed by the Health and Social Care Information Centre showed that in the West Midlands in 2010-11 there were 456 children under the age of 10 admitted to hospital with tooth decay.
In 2013-14 a “shocking” 1,444 were admitted.
Experts blame the trend on a culture of parents rewarding children with sweets while failing to clean their teeth properly as infants.
Dr Carter said: “The rise is absolutely incredible and is indicative of a massive failure in parenting.
“Partly it’s down to background and people from lower socio-economic groups have higher levels of tooth decay.
“It has to be about parenting and looking after children.
“In many cases the first time the child has ever seen a dentist is when they’re taken there in great pain.
“Basically if it gets as far as needing to go to hospital for general anaesthetic then you’re talking about multiple extractions.
“It’s not unusual for a child to have 12 to 14 teeth taken out and in some cases we’ve heard of all 20 baby teeth being removed.”
In 2010-11 120 under-fours were admitted to hospital for surgery in the West Midlands. This had rocketed 353 last year.
One theory for the rise in childhood tooth decay in the last three years is rising immigration of people from Eastern Europe, who are moving over with their families and receiving treatment on the NHS.
Three years ago the total number of people under the age of 19 needing to go to hospital for surgery was 996. Last year it was 2,074.
In 2010-11 there were 6,000 hospital admissions for tooth decay in the West Midlands of all ages. In 2013-14 that had risen to 7,883.
The move away three square meals a day can also be blamed for the growing problem, said Dr Carter.
Dr Carter said: “Children are now having seven to 10 ‘grazing’ meals, many of which are full of sugar.
“Studies have shown that if you put a spread of food in front of children they would chose to eat a balanced diets.
“But we have the problem where sweets are given as a reward and so they are identified as such by the children.”
Source: www.coventrytelegrap…
Section 7 Scotland’s Successful Childsmile Oral Health Programme
Evidence from New Zealand (2015)

COMPARISON of Age 5 Children:
|
In 20 years, Scotland’s rate of dental fillings* For age 5 children has been cut by more than half (2.93 to 1.27).
|
New Zealand’s rate of dental fillings for age 5 children unfortunately has INCREASED in this time, from 1.71 to 1.88 average fillings per child |
|
Since CHILDSMILE began, the rate of age 5 Scottish children FREE of decay has gone from 45% to 68%, national average. This is an improvement of 23%.
|
NZ has improved only by 3% in this time. Now at 57%, we are far behind Scotland. |
|
High decile areas of Scotland now have 83% of Children FREE of decay. |
Nowhere in NZ comes even close to this. Our top rated areas are non-fluoridated Wairarapa & Waitemata (76% & 72%). |
COMPARISON of Year 8 children:
|
Since CHILDSMILE began, Scotland’s rate of fillings* for Year 8 children has also been cut by more than half. |
Year 8 Kiwis have nearly twice as many fillings |
|
In 20 years, the rate of Scottish Year 8 children FREE of decay has almost doubled. |
NZ has improved only by 5% in this time. It is now 54% which lags far behind Scotland. |
* Refers to fillings, decayed and missing teeth
The Scottish Government has refused to initiate water fluoridation programmes in 2004 and has now rolled out “Childsmile” throughout Scotland. “Childsmile” is reported as being highly successful and note that this success has been used by activists in New Zealand to urge the discontinuation of fluoridation on the grounds that fluoride is not reducing dental decay at the same rate that Childsmile has recently reduced decay in Scotland.
Childsmile, Scotland compared with New Zealand which has water fluoridation.
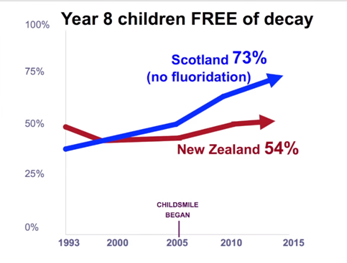
(Notice how New Zealand’s dental decay rate for Year 8 children has not improved since 1993.)
Source: www.youtube.com/watc…
Section 8 The Precautionary Principle
The precautionary principle enables rapid response in the face of a possible danger to human, animal or plant health, or to protect the environment. In particular, where scientific data do not permit a complete evaluation of the risk, recourse to this principle may, for example, be used to stop distribution or order withdrawal from the market of products likely to be hazardous.
Communication from the Commission on the Precautionary Principle (COM(2000) 1 final of 2 February 2000)
SUMMARY
The precautionary principle is detailed in Article 191 of the Treaty on the Functioning of the European Union (EU). It aims at ensuring a higher level of environmental protection through preventative decision-taking in the case of risk. However, in practice, the scope of this principle is far wider and also covers consumer policy, European legislation concerning food and human, animal and plant health.
This Communication establishes common guidelines on the application of the precautionary principle.
The definition of the principle shall also have a positive impact at international level, so as to ensure an appropriate level of environmental and health protection in international negotiations. It has been recognised by various international agreements, notably in the Sanitary and Phytosanitary Agreement (SPS) concluded in the framework of the World Trade Organisation (WTO).
Recourse to the precautionary principle
According to the European Commission the precautionary principle may be invoked when a phenomenon, product or process may have a dangerous effect, identified by a scientific and objective evaluation, if this evaluation does not allow the risk to be determined with sufficient certainty.
Recourse to the principle belongs in the general framework of risk analysis (which, besides risk evaluation, includes risk management and risk communication), and more particularly in the context of risk management which corresponds to the decision-making phase.
The Commission stresses that the precautionary principle may only be invoked in the event of a potential risk and that it can never justify arbitrary decisions.
The precautionary principle may only be invoked when the three preliminary conditions are met:
- identification of potentially adverse effects
- evaluation of the scientific data available
- the extent of scientific uncertainty
Precautionary measures
The authorities responsible for risk management may decide to act or not to act, depending on the level of risk. If the risk is high, several categories of measures can be adopted. This may involve proportionate legal acts, financing of research programmes, public information measures, etc.
Common guidelines
The precautionary principle shall be informed by three specific principles:
- the fullest possible scientific evaluation, the determination, as far as possible, of the degree of scientific uncertainty
- a risk evaluation and an evaluation of the potential consequences of inaction
- the participation of all interested parties in the study of precautionary measures, once the results of the scientific evaluation and/or the risk evaluation are available
In addition, the general principles of risk management remain applicable when the precautionary principle is invoked. These are the following five principles:
- proportionality between the measures taken and the chosen level of protection
- non-discrimination in application of the measures
- consistency of the measures with similar measures already taken in similar situations or using similar approaches
- examination of the benefits and costs of action or lack of action
- review of the measures in the light of scientific developments
The burden of proof
In most cases, European consumers and the associations which represent them must demonstrate the danger associated with a procedure or a product placed on the market, except for medicines, pesticides and food additives.
However, in the case of an action being taken under the precautionary principle, the producer, manufacturer or importer may be required to prove the absence of danger. This possibility shall be examined on a case-by-case basis. It cannot be extended generally to all products and procedures placed on the market.
Appendix A Explaining the Units when Discussing Fluoride
Using metric units, 1 litre of water weighs 1 kilogram.
This is a universal standard.
On the other hand, 1 litre of milk weighs more than 1 kilo because milk is denser than water.
In metric units, 1 milligram (mg) is one thousandth of a gram. 1 gram is one thousandth of a kilogram. Therefore, 1 mg is 1000 x 1000 = 1 millionth of a kilo.
When we talk about 1ppm we are describing 1 part in a million. That’s one-millionth of a litre.
With reference to water, since 1 mg is one-millionth of a litre, 1mg is the same thing as 1ppm.
‘Concentration’ is the word used to describe how much fluoride is in each litre of water. This is not the same as ‘dose’. A dose is the amount of fluoridated water drunk each day. The average dose is 2 litres water/day. However many people drink more. Therefore, the dose is uncontrolled.
The ‘optimum’ concentration of fluoride added to treated water in the UK is 1mg/litre of water or 1ppm. In the last few years, the USA and the Republic of Ireland have reduced the ‘optimum’ down to 0.7 – 0.8 ppm in order to reduce the widespread occurrence of Dental Fluorosis in permanent teeth. Hong Kong adds 0.5 ppm to drinking water. The UK has failed to follow suit. The reason for this failure is said to be “lack of evidence from monitoring data to support a variation of the target level for fluoride in drinking water.” (Hansard HL4593, 15th December 2015). This is a risible reply by the Government spokesperson since the evidence for dental fluorosis caused by fluoride is easily accessible from other countries.
The ‘optimum’ concentration was arbitrarily decided back in the 1940s in the USA. It was thought, with no credible research being done, that above this level children would get dental fluorosis (DF) whilst below this level there would be no protection for teeth from dental decay. We now know better!
Natural fluoride occurs in small isolated areas in the UK. Approx. 330,000 people drink this water. Natural fluoride is calcium fluoride (CaF2) but when in drinking water, the calcium and fluoride are in ‘free fall’. It’s only when the two elements are no longer in water (e.g. in the stomach as the water drains away) that the two elements bond and are no longer bioavailable.
5,797,000 people living in England purchase drinking water to which an artificially-produced fluoride compound has been added. That’s 10% of the population of the UK. Source: British Fluoridation Society’s publication One in a Million, 3rd ed., March 2012,
The fluoride atom in its electrically negative state (F–) is the same atom found in both natural and artificially-produced compounds. The other substances present in the fluoridating acid alter the way in which the body copes with fluoride.
Due to lack of research, there is lack of knowledge about the additive effects of combinations of the substances added to our drinking water when the fluoridating acid is added.
The fluoridating acid has many names. In UK Law, it’s known as hexafluorosilicic acid. It is more accurately called hydrofluorosilicic acid. The chemical formula for both is the same. H2SiF6. A laboratory analysis of the fluoridating acid added to drinking water in the Republic of Ireland detected 28 contaminants. (Fluoride, silica and hydrogen are in the chemical formula so there was no need to analyse the acid for these elements.)
Source: CAL Ltd analysis, Dublin, 14th August 2000. This analysis is not in the public domain. A copy can be provided.
The fluoridating acid added to English and Irish drinking water is a hazardous waste by-product which arises from the manufacture of phosphate fertiliser. The fluoridating acid used in Ireland originates in Spain whilst the English fluoridating acid originates in Finland.
Source: Wikipedia: en.wikipedia.org/wik…
It’s hazardous because the acid will form corrosive Hydrofluoric Acid (HF) which, when it evaporates, forms highly corrosive and toxic Hydrogen Fluoride gas (also HF).
The fluoridating acid used for water fluoridation is approximately a 20% solution. This means that:
20% is fluoride
76 – 76.5% is contaminated factory water which is used to ‘scrub’ the poisonous vapours out of the phosphate factory chimney
1.5% – 2% is hydrofluoric acid – or rather atoms of hydrogen and fluoride capable of forming hydrofluoric acid and hydrofluoric gas
2% is contaminants and silica – approx. 29 in no., depending on the origin of the ore used to manufacture phosphate fertiliser.
In order to add 1mg fluoride to each litre of treated water, it is necessary to add more than 5mg of the fluoridating acid to each litre. This little known fact is not admitted by the British Fluoridation Society in its publication One in a Million.
Source: YARA UK Guidelines – not in the public domain. A copy can be provided.
Although added to drinking water in minute quantities, many of the contaminants are bio-accumulative. Many have a synergistic effect in that their negative effects on our bodies are magnified when present in combination.
Hexafluorosilicic acid is not of British Pharmaceutical grade.
Appendix B Bioaccumulation and Bioavailability
It is well accepted that 50% of swallowed fluoride is excreted via the kidneys leaving 50% to bio-accumulate in the body. Why does the body reject 50% of the fluoride? The only explanation can be that calcium bonds with some of the fluoride and thus ‘escorts’ it out of the body. The remaining 50% of fluoride passes through the stomach lining or the lining of the ileum where it becomes strongly attracted to positive atoms such as in situ calcium and magnesium which are already ‘attached’ to bones and organs.
“Absorption of fluoride is rapid and extensive, with about 50% of the absorbed fluoride becoming associated with calcified tissues within 24 h and the remainder being excreted in the urine.” (Ref: ndt.oxfordjournals.o… )
Patients with Chronic Kidney Disease (CKD) will clear between 10% – 30% fluoride, leaving between 70% – 90% to bioaccumulate. Bioaccumulation takes places in bones. Recent research points to bioaccumulation in organs. In fact, wherever calcium is naturally deposited in the body, fluoride will also be found. Calcium fluoride is found in the pineal gland. (Luke, 1997, p. 168).
The sites of bioaccumulation are the bones, teeth and organs. Fluoride has been described as an avid bone-seeker.
“Physiologically, the fluoride ion is an avid bone seeker and a potent enzyme inhibitor.” (Burghstahler, 1977).
When there is calcium and magnesium present in the diet and stomach, then the bioaccumulation of fluoride is less.
Wakefield is supplied with water which contains 40-60 mg/litre of Calcium (100-150 Calcium carbonate) and therefore residents could be described as being moderately deficient in calcium. Any fluoride in the diet would bond with this calcium and prevent its bioavailability.
Ca+ and F – make a particularly strong bond in the body in the absence of water. This means that bonded fluoride cannot enter tooth material but at the same time calcium cannot be effective at helping the body in its numerous essential processes.
Appendix C The Nature of Fluoride and its Toxicity
Fluoride is fluorine gas but since fluorine cannot exist on its own in nature, it has to bond with another element. This means that the name of fluorine changes to fluoride to denote its dependence on bonding with another element for survival. Whenever we encounter fluoride, it’s shown as F–. This means that fluoride is fluorine with an extra electron meaning that the fluoride anion has an extra electro-negative (–) charge. (Electrons are negatively charged so the more electrons, the higher the negative charge. The chosen partner for bonding with fluoride is destined to be an element with a positive (+) charge.
Thus aluminium fluoride, calcium fluoride, magnesium fluoride and potassium fluoride: Al+F– , Ca+F2– , Mg+F– , K+F–
Fluoride is the most negatively charged of all the elements in the periodic table. This means that it packs a punch! As you move from left to right in the Periodic Table of the Elements (see next page), the negative reactivity of the elements increases. (The noble gases – far right – are not part of this sequence.)
Electro-negative elements attract positive elements. The more electro-negative elements attract the more positive elements. Thus Calcium+ is strongly attracted to Fluoride–.
The same is true of the attraction between magnesium and fluoride: Mg+F–.
British Standard (EN) 12175, lists a few of the contaminants in the fluoridating acid. The BSEN is not in the public domain and has to be purchased from the British Standards Institute. Extracts from the BSEN are as follows:
“Hexafluorosilicic acid is only stable in an aqueous solution. On evaporation it decomposes to hydrogen fluoride (HF) and silicon tetrafluoride (SiF4). It produces hydrogen on contact with metals, e.g. steel, nickel and aluminium. It is a strong acid [pH < 1] and reacts violently with alkalis. If forms hydrogen fluoride (HF) on contact with concentrated acids. It attacks glass. Hydrogen fluoride is present in the acid at a maximum of 1.5%. Chemicals present: antimony, arsenic, cadmium, chromium, lead, mercury, nickel, selenium. Other chemicals are not relevant because the raw materials used in the manufacturing process are free of them.”
[Comment: This final sentence seems to imply that the contaminants are in the acid but are not admitted to as being contaminants. However, the concentrations of these other contaminants may be quite high but there is no obvious legislation extant which protects our health against negative health effects of these contaminants in the fluoridating acid. According to EU law, though, it is not permissible to add hexafluorosilicic acid to food! (EU Reg. 1170/2009, UK Reg. 1631.2007 and EU Reg. 1925/2006). Water is food.
Periodic Table of the Elements
Inert Gases
<![if !vml]>![]() <![if !vml]>
<![if !vml]> Fluorine
Fluorine
Periodic Table of the Elements
<![if !vml]> <![if !vml]>
<![if !vml]>![]() <![if !vml]>
<![if !vml]> Magnesium (MG) Calcium (Ca) Potassium (K)
Magnesium (MG) Calcium (Ca) Potassium (K)
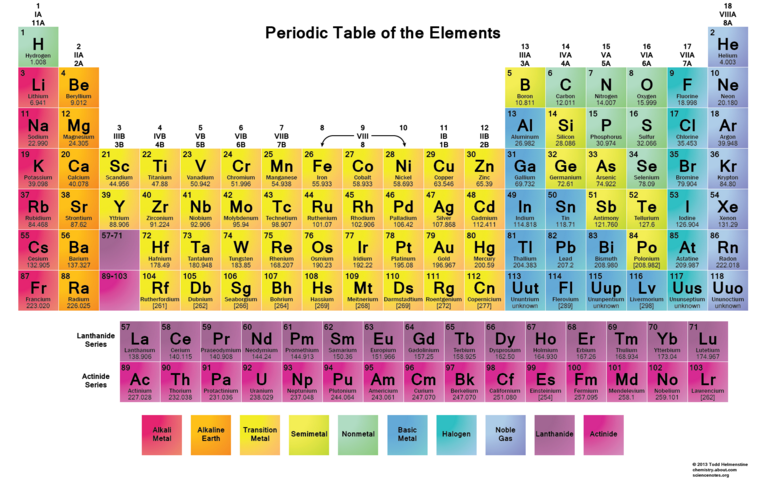
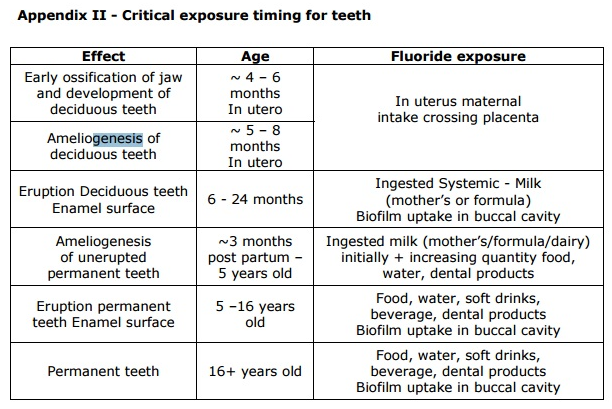
Avenues of exposure to fluoride
Source: ec.europa.eu/health/…
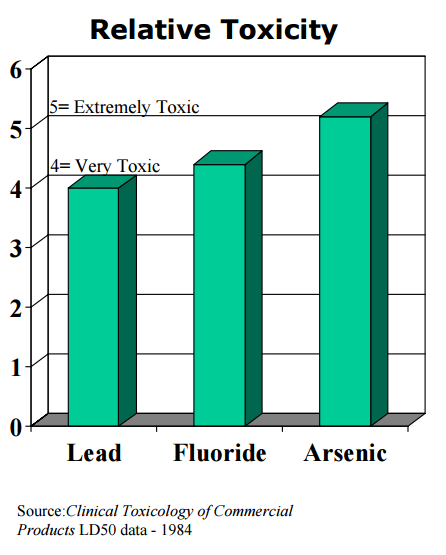
Appendix D The Negative Effect of Fluoride on Our Bodies
Fluoride: Damning New Evidence
Excerpted from “What Doctors Don’t Tell You”, March 1999
Researcher, Doris Jones, has unearthed startling new evidence demonstrating that fluoride interferes with enzymes, damaging many organs of the body.
The fluoride issue, a perennial hot potato, is heating up once again. In Britain, the government has recently announced its intention to fluoridate the water of deprived inner city areas, supposedly to improve the dental health of children living there. Later, water fluoridation may be introduced nationwide. A White Paper outlining the government’s plans is scheduled for the spring, 1999 (when-specific date).
The government and the dental profession have convinced the public that fluoridated water offers nothing but benefits-that there is overwhelming evidence that it prevents tooth decay and contributes to the strength of bones. There is tacit admission in the pro-fluoride camp that fluoride can also cause harm, but only at very high levels: 2 ppm in water may cause mottled teeth and 8 ppm may lead to bone disorders and degenerative changes in the vital organs.
A few lone voices have countered the prevailing view, with published evidence that fluoride can have devastating effects, causing mottled teeth and osteoporosis at very low levels. While much has been written about the effects of too much fluoride on teeth and bones, little is known about the effects of fluoride on the rest of the body. But new evidence has emerged demonstrating that it has devastating effects on just about every organ in the body, and may even be partly responsible for behavioural problems like hyperactivity and many puzzling illnesses like ME.
The late fluoride critic George L Waldbott discovered that, besides teeth and bones, fluoride can damage soft tissue. According to his research, the small fluorine ion with a high-charge density can combine with other ions and penetrate every cell in the body. It interferes with the metabolism of calcium and phosphorus and the function of the parathyroid glands. It has a strong affinity to calcium, but will also readily combine with magnesium and manganese ions and so can interfere with many enzyme systems that require these minerals. The interruption of these enzyme systems, in turn, may disturb carbohydrate metabolism, bone formation and nerve-muscle physiology. Indeed, every vital function in the body depends on enzymes; because fluoride easily reaches every organ, many diverse toxic symptoms can result.
“Most diseases are results of disturbances of the enzyme systems,” says Professor Abderhalden. “Damage due to fluoride could be shown on 24 enzymes.” Enzyme systems react to fluoride in different ways; some are activated, others are inhibited. Lipase (essential for the digestion of fat) and phosphatases are very sensitive to fluoride. In patients with skeletal fluorosis, succinate dehydrogenase activity is inhibited. In chronic fluoride poisoning, this diminished enzyme activity accounts for muscular weakness and even muscle wasting. Human salivary acid phosphatase is diminished by half when exposed to 3.8 ppm of fluoride, while blood enzyme cholinesterase is inhibited by 61 per cent on exposure to 0.95 ppm fluoride-a level within recommended levels So what does this do in the body? (Author, Handbook of Experimental Pharmacology, Springer Verlag, 1970: 48-97).
Alkaline phosphatase, an enzyme involved in bone growth and liver function, may also be poorly affected by low-level fluoride intake. According to scientists from the Department of Chemistry of the University of California at San Diego, fluoride switches off an enzyme by attacking its weakest links-the delicately balanced network of hydrogen bonds surrounding the enzyme’s active sites (J Biol Chem, 1984; 259: 12984-88).
Their particular studies concerned the enzyme cytochrome C oxidase, an oxygen-carrying respiratory enzyme; deficiencies of this vital enzyme have been linked to cancer, severe diseases and even cot death.
It’s also been shown by research at Kings College in London that fluoride forms very strong hydrogen bonds with amides, which are formed when amino acids join together to form a protein (J Am Chem Soc, 1981; 103: 24-8). This can also cause chromosomal damage. If the protein is greatly distorted, the body’s immune system no longer recognises it, treats it as a foreign protein and will try to destroy it, which in turn triggers allergic skin or gastrointestinal reactions (J Yiamouyannis, Fluoride: The Aging Factor,. Delaware, Ohio: Health Action Press, 1993: 94-9).
Stomach and bowel disorders are the main features of fluoride intolerance. Even small amounts of fluoride can form hydrofluoric acid in the stomach to produce gastric pains, nausea and vomiting. Young children are particularly at risk. Fluoride tablets can even cause gastric haemorrhages; in one instance, a 9-year-old boy sustained such damage that he required the removal of large parts of his stomach (Fluoride, 1977; 10: 149-51).
The most readily identifiable feature of soft-tissue fluorosis is extraordinary general fatigue, which is frequently linked to thyroid deficiency. The thyroid gland requires iodine to produce the hormone thyroxine, which controls the rate of metabolism in the body. But when fluorine is present, it displaces iodine, which will cause a thyroid gland to stop working properly (K Roholm: Fluor and Fluorverbindungen, in: Handbuch Experimenteller Pharmakologie, Ergaenzungswerk, Vol.7, Springer, 1938: 20).
The parathyroid gland, which regulates the distribution of calcium and phosphorus in the body, is extremely sensitive to excessive amounts of fluoride. Over fifty years ago, Indian clinicians found a close relationship between skeletal fluorosis and hyperparathyroidism (J Hyg 1942; 42: 500-4).
Fluoride has even been shown to affect the pituitary gland, which controls growth rate by regulating the production of thyroid hormones (Seances Soc Biol Fil, 1930; 103: 981-2). In animals, less than normal amounts of thyroid hormones are produced when animals are given water containing a fluoride content equivalent to that of artificial water fluoridation (Bull Schweiz Akad Med Wiss, 1954; 10: 211-20). Using scanning electron-microscope photographs, Professor AK Susheela of the Fluoride and Fluorosis Research Foundation of India and Senior Consultant to the Indian government, who has published over 100 scientific papers on the hazards of fluoride, proved that when exposed to fluoride, red blood cells are killed prematurely, lowering haemoglobin and causing anaemia.
She also showed that calcium levels diminish as fluoride levels in the body rise; the gastrointestinal tract mucosa is damaged, causing irritable bowel syndrome; and blood fluoride levels rise continuously with prolonged use of fluoridated toothpaste.
When people are bombarded with fluoride, in the form of fluoridated water, toothpaste and mouth rinses, muscles and elements of connective tissue, particularly collagen fibre and bone tissue, undergo degenerative changes.
At the 1998 US Conference of the International Society for Fluoride Research in Bellingham, Washington, Dr Jennifer Luke from the University of Surrey, UK, presented evidence on the effects of low and high doses of fluoride on the pineal gland in gerbils. In both gerbils and humans this gland helps control the aging process and the production of melatonin, which regulates the sleep/wake cycle. Gerbils exposed to a high level of fluoride experienced a significant decrease in the production of melatonin, and earlier genital maturation. While animal studies may not always be applicable to humans, Dr Luke theorised that mass fluoridation may be behind the general decline in the age of puberty in the West (Fluoride, 1998; 31: 4: 175).
In areas where water is fluoridated, evidence shows that dangerously high fluoride concentrations accumulate in many soft tissues and organs of the population, including the heart, kidney and bladder; the highest level ever recorded-8400 ppm-was found in the aortas of people living in Grand Rapids, Michigan, where fluoride was first introduced in America.
The heart and blood vessels are affected by fluoride. Cardiac irregularities and low blood pressure have been noted in experimental poisoning using large doses (Publ Health Report, 1956;71:459-67). In 1950, five years after experimental introduction of fluoride into drinking water in Grand Rapids, Michigan, the number of deaths from heart disease nearly doubled (The Grand Rapid Herald, July 28, 1955). Death rates due to cancer, intracranial lesions, diabetes and arteriosclerosis were all markedly increased compared to death rates per 100,000 in the entire state.
In electrographic studies, Japanese researcher Taka Mori showed a direct link between damage to the heart and dental fluorosis in children who drank water with a fluoride content of 0.5-6.2 ppm. Fluoride also affects arteries, causing bruise-like skin lesions called “Chizzola maculae'”, showing inflammatory areas around capillary blood vessels. Because fluoride attracts calcium, it contributes to their hardening.
Fluoride affects the brain and entire central nervous system. Neurological problems like headaches, vertigo, spasticity in extremities, visual disturbances and impaired mental acuity can all result. Tissue damage to anterior horn cells has been found (Fluoride,1975;8:61-85). Official annual statistics revealed that death rates among malnourished children in the Chilean town of Curico, fluoridated since 1953, were to 104 per cent higher than in comparable, non-fluoridated towns, and the general mortality was higher by 113 per cent, compared with the average for the country (Ziegelbecker R et al, Journal? 1995:47-48).
Fluoride, hyperactivity and violence
Several studies have shown that exposure to fluoride can cause behavioural changes (Int Clin Psychopharmacol, 1994;9:79-82; Neurotoxicol and Teratol, 1995;17:169-77; Fluoride, 1996;29:187-88) At a 1998 Conference on Fluoride, Professor Roger Masters reported a link between the blood lead levels of 280,000 children in Massachusetts and the use of silicofluorides for water fluoridation. Here and in Georgia, behaviours associated with lead toxicity, such as violent crime, are more frequent in communities using silicofluorides than in areas not using them. At the same conference Dr Phyllis Mullenix reported results of a study using two steroids to treat childhood leukaemia, one of which had a fluorine atom in its structure. In the study, this steroid caused behaviour patterns typical of hyperactivity. A follow-up study of children using this drug for two years showed a significant drop in average IQ scores, compared with children using the non-fluoride drug (Fluoride, Nov.1998;31;4:175).
In one family in Glasgow, every member is severely affected by fluoride-the mother experienced an anaphylactic shock to Prozac, which contains fluorine, and all four children exhibited erratic/violent behaviour and suffered from immune system damage on exposure to fluoride (in their drinking water?
Fluoride and ME
Although few researchers have looked at the role of fluoride in the development of ME, there are conspicuous similarities between key features of ME/CFS and those seen in the very early stages of chronic fluoride intoxication (Fluoride,1998; 31:13-20)
Dr John McLaren Howard of Biolab in London offers a few important clues why. He discovered that ME patients experience reduced movement of white blood cells when exposed to quite low levels of fluoride (InterAction 14, Autumn, 1994:53-54). This effect on white blood cells might render patients less able to fight infections efficiently, or lead to an exacerbation of their health problems.
Fluoride also interferes with phagocytosis ,as well as causing the release of superoxide free radicals in resting white blood cells. This means that fluoride slows down and weakens the very cells which serve as the body’s defence system; bacteria, viruses, chemicals and the body’s own damaged or cancerous cells are then allowed to wreak havoc. Minor infections take longer to throw off and cause more serious illness (John Yiamouiannis, The Aging Factor, Health Action Press, 1993:p32). This is precisely what appears to be happening in many cases of ME.
We do not know how many children or teenagers had topical high concentration fluoride dental treatment before succumbing to infections which led to ME/CFS. My son had fluoride treatment to prevent tooth decay in the autumn of 1979, after which his health dramatically deteriorated, commencing with gastric problems, various minor infections, then glandular fever, followed by atypical measles, more infections and eventually resulting in ME in 1980. In the end the fluoride treatment didn’t work in preventing tooth decay-he’s needed 15 fillings over the past nine years.
The American pathologist Majid Ali explains that chronic fatigue results due to “accelerated oxidative molecular injury”. Only a well functioning enzyme system can protect us from such injury and maintain normal energy levels. In chronic fatigue there is a high frequency of membrane deformities, due to increased oxidative stress on the cell membranes, which is why sufferers lack energy. Interestingly, Ali also highlights gastrointestinal disturbances, such as IBS, as playing a significant part in chronic fatigue (The Canary and Chronic Fatigue, Life Span Press, 1994).
Many ME patients have an underactive thyroid (InterAction 27, Sept.1998:27). Chronic fatigue and exhaustion due to hypothyroidism is a cardinal feature in the Chronic Fluoride Toxicity Syndrome.
Experienced researchers who have studied ME for decades maintain that as with polio, it is damage to anterior horn cells caused by a gut virus, which explains why polio victims are paralysed or suffer from impaired motor function (The Clin and Scientific Basis of ME/CFS). But fluoride has also been shown to damage anterior horn cells . Gastrointestinal disturbances, often referred to as IBS, are also known to play a significant part in ME, as they are in the Chronic Fluoride Toxicity Syndrome.
Severe sleep disturbances, or reversal of sleep rhythm, are a common feature in ME/CFS (Clin). Deposits of large quantities of fluoride in the pineal gland of animals have caused similar problems (J Luke, Bellingham Conference, 1998).
At this point, no one knows to what extent these syndromes overlap, or fluoride or fluorine facilitates the development of ME by various biological agents. The indications are that fluoride may act as as a “facilitating co-factor” and exacerbate existing problems in such patients. Or it could be, as Dr H C Moolenburgh suggests, that ME is one of the end stages of a general chemical poisoning, with fluoride one of the worse offenders (personal communication, 7.1.1999). Although many unanswered questions remain, one thing can be said with certainty. Fluoride not only is not beneficial, but may turn out to be one of the major factors in the serious health problems besetting modern man.
Doris Jones
© What Doctors Don’t Tell You Ltd. 1999
Source: www.nofluoride.com/w…
Damning new evidence
Appendix E. YARA UK Guidelines for the Handling of Hexafluorosilicic Acid
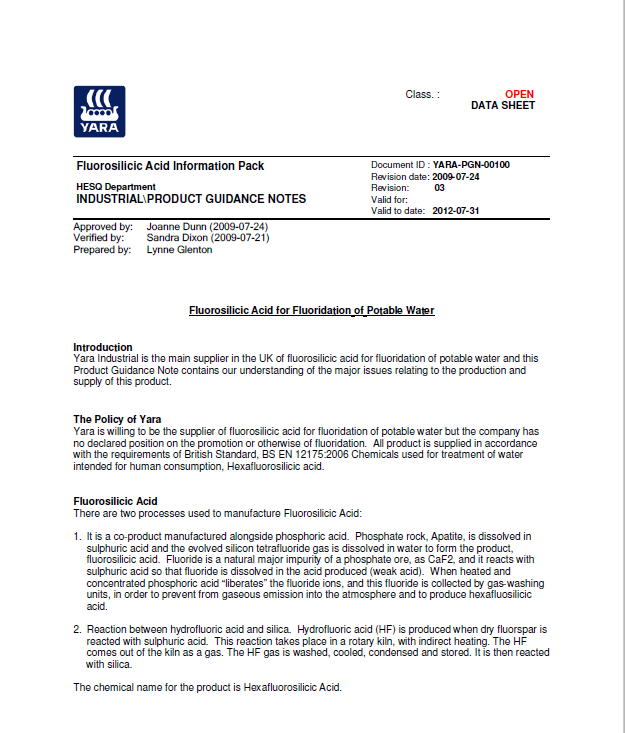
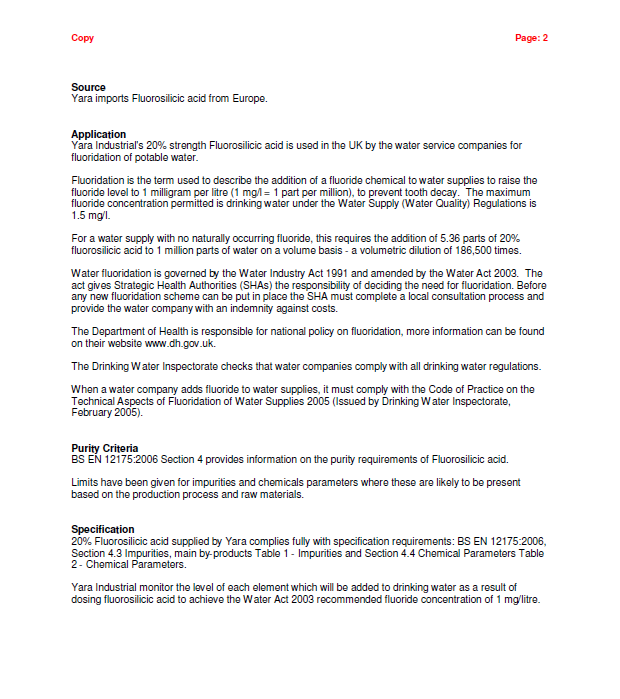
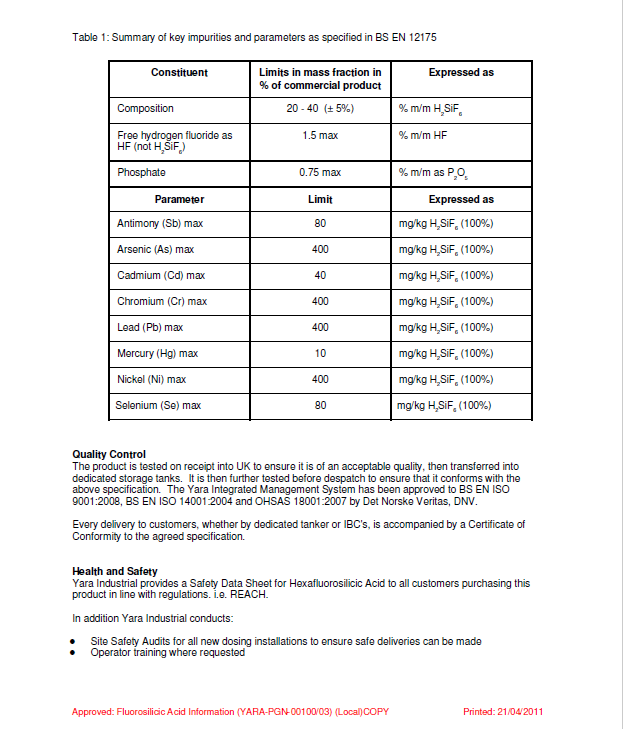
Page 4 was redacted by YARA UK
Appendix F CAL Laboratory Analysis of Hexafluorosilicic Acid